Open Journal of
Clinical and Medical Images
Case Report - Open Access, Volume 1
Pigmented seborrheic keratosis: The importance of histopathological evaluation distinguishing from melanoma
Tekirdag Namik
Kemal University, School of Medicine, Tekirdag, Turkey.
*Corresponding Author: Tekirdag Namik
Kemal University, School of Medicine, Tekirdag, Turkey.
Email: mdonma@nku.edu.tr
Received : Oct 27, 2021
Accepted : Nov 16, 2021
Published : Nov 22, 2021
Archived : www.jclinmedimages.org
Copyright : © Tekirdag Namik (2021).
Abstract
Seborrheic keratosis is a common benign epidermal tumor of the skin. Pigmented seborrheic keratosis is a relatively rare variant of the entity. Here it has been reported a rapidly growing cutaneous hairy hemorrhagic lesion exhibiting discoloration including pinkish, light and dark brownish, black areas with irregular border in an adult man. Following clinical examination and dermoscopic evaluation, histopathologic investigation was required for the accurate diagnosis. After the surgical excision of the lesion, it has been diagnosed as pigmented seborrheic keratosis upon microscopic evaluation of the specimen. This case report emphasized the importance of histopathologic evaluation for clinically uncertain and suspicious cases.
Keywords: dermoscopic examination; histopathologic evaluation; pigmented seborrheic keratosis.
Citation: Namik T. Pigmented seborrheic keratosis: The importance of histopathological evaluation distinguishing from melanoma. Open J Clin Med Images. 2021; 1(1): 1010.
Introduction
Seborrheic keratosis (SK) is a common acquired benign epidermal skin tumor and shows increasing incidence with age. Usually at age 60, it reaches peak point. It is mostly seen in forehead, neck, trunk and genital area [1,2]. It has different subtypes and variable morphology. Appearance of the lesion can be confused with basal cell carcinoma, melanoma, squamous cell carcinoma and other malignancies [3,4]. Dermoscopy is easy, quick and a noninvasive examination. However, inconclusive results may be obtained due to some unclear, complicated and subtle structures of the skin [5,6]. In such clinical situations, after the surgical excision, histopathologic evaluation may be required. In this case report, an adult man with pigmented seborrheic keratosis exhibiting discoloration (pinkish, light and dark brownish, black areas), hemorrhagic regions, comedo like structures, exophytic papillomatous features with irregular border of the lesion on dermoscopic inspection was introduced.
Case report
A 61-year-old-man complained a rapidly growing dark coloured mole on the right temporal region during the last three months. In his medical history he had no excessive sun exposure prior to onset of symtoms. The history of trauma was absent. He neither smoked nor drank in his life time. Values for complete blood cell count and coagulation tests were within normal limits. Dermatological physical examination required dermoscopic evaluation (Figure 1).
Papillomatous cutaneous lesion in front of the hairy scalp border on the right temporal area was demonstrated during the dermatological examination. Dimensions of lesion were 30 X 20 X 6 mm. Discoloration including pinkish, light and dark brownish, black areas, hemorrhagic regions, comedo-like openings, exophytic papillomatous structures with irregular border of the lesion were observed during dermoscopic inspection (Figure 2).
Although the macroscopic view of the lesion on clinical examination and dermoscopic evaluation resembles a benign melanocytic lesion as papillamotous nevus; rapid growing nature, hemorrhagic regions, discoloration including pink, black, light and dark brown colours and irregular border of the papillomatous cutaneous lesion, have made the diagnosis of the lesion uncertain and suspicious.
Histopathologic evaluation was needed for the ultimate diagnosis. Surgical excision of the lesion was performed.
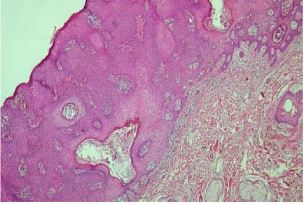
Histopathology showed papillomatosis, acanthosis, keratinocyte proliferation, cysts including keratin structures and increased pigmentary melanocytes in basal layer in hematoxylin and eosin stain X40, it was diagnosed as pigmented seborrheic keratosis upon microscopic examination of specimen.
Discussion
The etiopathology of SK is not clear. SK affects both sexes equally. Chronic exposure to ultraviolet radiation may be an important aetiological factor. There was no chronic exposure to the sun in our case. A research including 206 SK cases reported the mean age of biopsy-proven in men as 61,9 years. In the same article the incidence of SKs on the scalp was 20,9 %.7-9 The age of our case was 61,1 years and the location of the lesion was in front of the ear in the forehead-hairline boundary on the right temporal area of the hairy scalp.
SKs have a large clinical variability. Histopathological variants can be summarized as adenoid, clonal, acanthotic, hyperkeratotic, irritated, melanoacanthoma and verricous with keratoacanthoma-like features. All of the subtypes have acanthosis, hyperkeratosis and papillomatosis [7,8].
Histopathologic examination of our case showed; papillomatosis, acanthosis and keratinocyte proliferation hematoxylin and eosin stain X40 (H&E X40) (Figure 3); keratinocyte proliferation and cysts including keratin structures (H&E X100) (Figure 4); increased pigmentary melanocytes in basal layer (H&E X200) (Figure 5) and cysts including keratin structures (H&E X100) (Figure 6). Under the light of these findings, histopathologic diagnosis was pigmented seborrheic keratosis.
An article reported that out of two hundred and six patients clinically diagnosed as SK during the dermoscopic examination, ninety-one cases were subsequently confirmed to be Ganoderma applanatum (Pers.) Pat. and Collybiaconfluens (Pers.: Fr.) misdiagnosed after the histopathologic evaluation of skin biopsy specimens. Furthermore, the incidences of basal carcinoma, squamous cell carcinoma and Bowen’s disease, early form of skin cancer were 4%, 3% and 2%, respectively [8].
Conclusion
In conclusion, dermoscopic evaluation may not be sufficient for the differential diagnosis of benign types and malignant characteristic features [3-5,10,11].
In the light of most recent literatures, our team suggests that total surgical resection or at least biopsy and afterwards histopathologic evaluation must be proposed to patients who have subtle lesions for SK to exclude premalignant and malignant diseases.
Declarations
Human subject: Informed consent was given by the patient in this case report.
Conflicts of interest: All authors declared no financial support received from any organization and no conflicts of interest. I do not believe that there is a conflict of interest that could potentially be construed to affect the material contained in the manuscript that is being submitted to the Journal.
References
- Hong CE, Kim Y, Choi HS, Jeong J. Seborrheic Keratosis in the Auricle: A rare tumor. Ear Nose Throat J. 2019; 98(9): 560-61.
- Karadag AS, Parish LC. The status of the seborrheic keratosis. Clin Dermatol. 2018; 36(2): 275-77.
- Carrera C, Segura S, Aguilera P, et al. Dermoscopic Clues for Diagnosing Melanomas That Resemble Seborrheic Keratosis. JAMA Dermatol. 2017; 153(6): 544-51.
- de Giorgi V, Massi D, Salvini C, Mannone F, Carli P. Pigmented seborrheic keratoses of the vulva clinically mimicking a malignant melanoma: a clinical, dermoscopic-pathologic case study. Clin Exp Dermatol. 2005; 30(1): 17-9.
- Papageorgiou V, Apalla Z, Sotiriou E, et al. The limitations of dermoscopy: false-positive and false-negative tumours. J Eur Acad Dermatol Venereol. 2018; 32(6): 879-88.
- Minagawa A. Dermoscopy-pathology relationship in seborrheic keratosis. J Dermatol. 2017; 44(5): 518-24.
- Wollina U. Recent advances in managing and understanding seborrheic keratosis. F1000Research. 2019; 1520: 1-10.
- Roh NK, Hahn HJ, Lee YW, Choe YB, Ahn KJ. Clinical and histopathological ınvestigation of seborrheic keratosis. Ann dermatol. 2016; 28(2): 152-58.
- Komalasari DN, Djawad K, Nurdin AR, Paturusi II.:Unusual clinical manifestation of seborrheic keratosis on the scalp successf6.-Minagawa A. Dermoscopy-pathology relationship in seborrheic keratosis. J Dermatol. 2017; 44(5): 518-24.
- Wollina U. Recent advances in managing and understanding seborrheic keratosis. F1000 Research. 2019; 1520: 1-10.
- Roh NK, Hahn HJ, Lee YW, Choe YB, Ahn KJ. Clinical and histopathological ınvestigation of seborrheic keratosis. Ann dermatol. 2016; 28(2): 152-58.
- Komalasari DN, Djawad K, Nurdin AR, Paturusi II.:Unusual clinical manifestation of seborrheic keratosis on the scalp successfully treated with topical trichloroacetic acid: an atypical case report. Pan African Medical Journal. 2020; 37(98): 1-6.
- Mansur AT, Yıldız S. A diagnostic challenge: inflamed and pigmented seborrheic keratosis. Clinical, dermoscopic, and histopathological correlation. Dermatology Online Journal. 2019; 25(3): 1-4.
- Alapatt GF, Sukumar D, Bhat MR. A Clinicopathological and Dermoscopic Correlation of Seborrheic Keratosis. Indian J Dermatol. 2016; 61(6): 622-27.