Open Journal of
Clinical and Medical Images
Case Report - Open Access, Volume 1
Bilateral superficial optic disc drusen: A case report and literature review
Ke Xiong
Department of Ophthalmology, Nanfang Hospital, Southern Medical University, No. 1838 Guangzhou Avenue North, Guangzhou, Guangdong, 510515, China
*Corresponding Author: Ke Xiong
Department of Ophthalmology, Nanfang Hospital, Southern Medical University, No. 1838 Guangzhou Avenue North, Guangzhou, Guangdong, 510515, China
Email: shinco1223@163.com
Received : Nov 09, 2021
Accepted : Nov 30, 2021
Published : Dec 03, 2021
Archived : www.jclinmedimages.org
Copyright : © Xiong k (2021).
Abstract
We herein report a relatively rare case of bilateral superficial optic disc drusen in 50-year-old woman who complained of binocular visual field defects. She did not have any loss of vision, photophobia, tears, ophthalmodynia, headache, or other symptoms of discomfort. At the first visit, the direct ophthalmoscopy appears an optic disc elevated having a nodular appearance and blurred optic disc margins. And then, thought various examination methods such as B-ultrasound, visual field test, FFA, OCT, and MRI, it was clearly diagnosed as bilateral superficial optic disc drusen. There is no standard treatment for optic disc drusen, and observation is usually the preferred option. This case just was treated with vasoactive agents. Close follow-up was ongoing at the time of this writing.
Keywords: optic disc drusen; superficial drusen; optical coherence tomography.
Citation: Xiong K. Bilateral superficial optic disc drusen: A case report and literature review. Open J Clin Med Images. 2021; 1(1): 1015.
Introduction
Optic disc drusen (ODD) is acellular deposits of calcium, amino, and nucleic acids and mucopolysaccharides, formed in the prelaminar optic nerve head. ODD is just an incidental finding in ophthalmological practice. It can be classified as superficial or buried [1]. The prevalence of ODD ranged from 0.4 to 3.7% of the overall population, especially buried. Most cases are bilateral and occur in Caucasians in a higher prevalence, Asians are rare [2,3].
Superficial ODD is often visible in direct ophthalmoscopy, with an optic disc elevated having a nodular appearance and blurred optic disc margins without obscuration of peripapillary retinal vessels [4]. There is a correlation between superficial ODD and visual field defects. On the contrary, buried ODD does not have the typical nodular aspect, which is hardly directly seen through ophthalmoscopy, making it difficult to distinguish it from papilloedema. Buried ODD often is asymptomatic, do not affect vision and visual field [5].
Case report
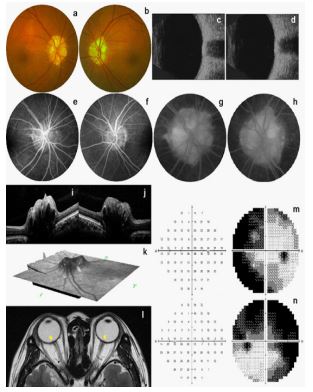
A 50-year-old female patient complained of binocular visual field defects. Ophthalmological examination: visual acuity testing of both eyes was 20/20. Ocular motility and slit-lamp examination of the anterior segment were within a normal range. An optic disc elevated having a nodular appearance and blurred optic disc margins in direct ophthalmoscopy. B-scan ultrasonography appears it has highly reflective round structures with posterior acoustic shadowing. Fluorescein angiographic shows nodular disc staining, no fluorescein leakage. OCT images show a hyperreflective irregular anterior margin. Posteriorly the margin is less evident due to signal blockage. MRI imaging appears as an abnormal signal on the disc, but optic nerve is well. Visual field test shows peripheral visual field defects, nasal defective visual field in the right eye and nasal and supratemporal defective visual field is the left eye (Figure 1).
Diagnosis: bilateral superficial optic disc drusen.
This study was approved by the Nanfang Hospital of Southern Medical University Medical Ethics Committee review board. Informed written consent was obtained from the patient for publication of this case report and accompanying images.
Discussion
We describe the results of a bilateral superficial optic disc drusen. The aetiology of ODD is still not clear, and it may be based on an abnormal axonal metabolism, consequent axonal disruption, and extrusion of mitochondria into the prelaminar extracellular space with the dysregulation of calcium deposition. The ODD has been also associated with dysplastic discs or abnormal disc vasculature, the calcified drusen may be related to hypocalcemic state. Both sporadic occurrence and autosomal dominant inheritance have been reported [6,7].
The typical characteristics of ODD is an optic disc elevated having a nodular appearance [8]. ODD diagnosis is made by ultrasound, FFA, CT or MRI, OCT, and so on. B-scan ultrasonography appears it has highly reflective round structures. Fluorescein angiographic shows nodular disc staining. CT or MRI imaging appears as an abnormal signal on the disc, but it is not obvious. OCT images can clearly see the appearance of ODD [9-12].
ODD is often considered a benign disease, but the majority of patients with a superficial ODD present with visual field defects and have a higher risk of developing anterior ischemic optic neuropathy (AION). Visual Field defects are common but not occur in the majority of patients, thus in variable percentage between series 24% to 87%. This patient complained of visual field defects. The reports of visual field tests show moderate or severe peripheral visual field defects in both eyes. This is due to the gradual enlargement of the wart body, the decrease of capillaries around the optic nerve, and the decrease of blood vessel density, which makes nerve fiber ischemia a possible mechanism for thinning of retinal nerve fibers around the optic papilla and related visual field changes [13,14].
To the best of our knowledge, there is no standard treatment for ODD, and observation is usually the preferred option. In order to reduce the compression of the optic nerve fibers, radial neurotomy has been proposed; however, this surgical procedure is not currently recommended due to the high surgery-related risks and the absence of a proven benefit. However, in the case of progressive visual field defects, it has been argued that intraocular pressure-lowering drops and vasoactive agents might help ODD improve optic nerve head perfusion [15,16]. This case was treated with vasoactive agents, being followed up.
Conclusion
Bilateral superficial optic disc drusen is relatively rare and can be clearly diagnosed by various examination methods such as fundus, B-ultrasound, Visual field test, FFA, OCT, and MRI. However, Due to ODD is smaller, the spatial resolution of MRI is not enough to detect ODD. Because of OCT has the advantages of high resolution and non-invasive, OCT specially swept source or enhance-deep imaging are the best methods to diagnose and locate ODD.
Declarations
Conflict of interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Friedman AH, Beckerman B, Gold DH, et al. Drusen of the optic disc. Surv Ophthalmol. 1977; 21: 373-390.
- Ghassibi MP, Chien JL, Abumasmah RK, et al. Optic nerve head drusen prevalence and associated factors in clinically normal subjects measured using optical coherence tomography. Ophthalmology. 2017; 124: 320-325.
- Rotruck J. A review of optic disc drusen in children. Int Ophthalmol Clin. 2018; 8: 67-82.
- Allegrini D, Pagano L, Ferrara M, et al. Optic disc drusen: a systematic review: Up-to-date and future perspective. Int Ophthalmol. 2020; 40: 2119-2127.
- Razek A, Batouty N, Fathy W, et al. Diffusion tensor imaging of the optic disc in idiopathic intracranial hypertension. Neuroradiology. 2018; 60: 1159-1166.
- Tso MO. Pathology and pathogenesis of drusen of the optic nervehead. Ophthalmology 1981; 88: 1066-1080.
- Mănoiu MR, Amri JA, Țicle A, et al. Case report: bilateral opticnerve head drusen and glaucoma. Rom J Ophthalmol 2017; 61: 310-314.
- Pineles SL and Arnold AC. Fluorescein angiographic identification of optic disc drusen with and without optic disc edema. J Neuroophthalmol. 2012; 32: 17-22.
- Malmqvist L, Lund-Andersen H, and Hamann S. Long-term evolution of superficial optic disc drusen. Acta Ophthalmol. 2017; 95: 352-356.
- Malmqvis L, Bursztyn L, Costello F, et al. The optic disc drusen studies consortium recommendations for diagnosis of optic disc drusen using optical coherence tomography. J Neuroophthalmol. 2018; 38: 299-307.
- Sato T, Mrejen S, and Spaide RF. Multimodal imaging of optic disc drusen. Am J Ophthalmol. 2013; 156: 275-282.e1.
- Gise R, Gaier ED, and Heidary G. Diagnosis and imaging of optic nerve head drusen. Semin Ophthalmol. 2019; 34: 256-263.
- Hamann S, Malmqvist L, and Costello F. Optic disc drusen: understanding an old problem from a new perspective. Acta Ophthalmol. 2018; 96: 673-684.
- Biçer Ö and Atilla H. Microvascular changes associated with optic disc drusen: case report. Turk J Ophthalmol. 2019; 49: 300-304.
- Jirásková N and Rozsíval P. Results of 62 optic nerve sheath decompressions. Cesk Slov Oftalmol. 1999; 55: 136-144.
- Nentwich MM, Maertz J, and Rudolph G. Optic disk drusen: historical and up-to-date aspects. Klin Monbl Augenheilkd. 2016; 232: 257-265.