Open Journal of
Clinical and Medical Images
Clinical Image - Open Access, Volume 2
Intra-articular ganglionic cyst of anterior cruciate ligament: A very rare entity
Rajaram Sharma
Department of Radio-Diagnosis, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
*Corresponding Author: Rajaram Sharma
Department of Radio-Diagnosis, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
Email: hemantgalaria13@gmail.com
Received : Dec 28, 2021
Accepted : Jan 27, 2022
Published : Jan 31, 2022
Archived : www.jclinmedimages.org
Copyright : © Sharma R (2022).
Citation: Sharma R. Intra-articular ganglionic cyst of anterior cruciate ligament: A very rare entity. Open J Clin Med Images. 2022; 2(1): 1024.
Description
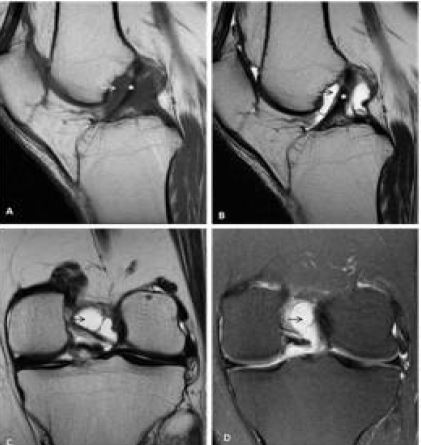
A 27-year male presented to our orthopaedic department with complaint of pain in left knee joint on long standing or running since three months. The pain increased with deep flexion. There was no history of trauma or any systemic illness. He was advised X-ray of the left knee joint, which turned out to be normal. For further evaluation, he underwent multiparametric MRI scan of the left knee. MRI demonstrated a well-defined, round to oval, lobulated, loculated abnormal intensity lesion measuring about 17 X 16 X 23 mm in the inter-condylar notch adjacent to ACL. The lesion appears hypointense on T1WI, hyperintense on T2WI and proton density fat saturation (PDFS) sequence.(Figure 1). The lesion is seen extending posterosuperiorly in the intercondylar notch (Figure 2). The diagnosis of ACL cyst was made, and the patient was prescribed analgesics along with rest. He had near complete resolution of his symptoms in the next follow up and no signs of any recurrence till the writing of this article.
A ganglionic cyst is an umbrella term for a wide range of histologic diagnosis. An intra-articular ganglionic cyst is a rare finding, often found incidentally. ACL ganglionic cysts have an incidental detection rate of about 1.3% on magnetic resonance imaging (MRI) [1]. There are several theories regarding the pathogenesis of ACL ganglion cysts like degenerative changes in connective tissue after trauma, herniation of synovial tissue and synovial tissue ectopia. Most of the ACL cysts are asymptomatic, but the patient may present with pain in the knee, restriction of movements, swelling around the knee and knee locking [2]. If symptomatic, these are usually resected with a very low rate of recurrence. On MRI, the ganglionic cyst appears hypointense on T1 weighted images (T1WI) but maybe slightly hyperintense when there is high proteinaceous content or haemorrhage within the ganglia. On T2/STIR, these ganglia have high signal intensity. The choice of treatment usually depends on the severity of symptoms. The asymptomatic patients or less severe symptoms are better left untreated. Surgical interventions include ultrasound (USG) / computerized tomography (CT) guided aspiration or open surgeries [3].
Learning points
- ACL ganglionic cysts are an incidental finding but an important differential in the causes of chronic knee pain.
- ACL ganglionic cysts can resolve with conservative measures, but surgical excision is the treatment of choice.
- MRI is the modality of choice for the diagnosis of this entity.